ROYAL COMMISSION: An overuse of medications and restrictive practices
The Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability held hearings, running from 22 – 25 September, examining the use of psychotropic medication to address behaviours of concern exhibited by people with disability.
Kate Eastman SC, Senior Counsel Assisting the Royal Commission, acknowledged that this hearing would have a lack of people with disability sharing their stories about the use of chemical restraint.
Ms Eastman says, “People who have been subjected to chemical restraints are not always able or willing to speak about their experiences, and this has had consequences for this public hearing. And the absence of people with disability who have experienced chemical restraints speaking for themselves in this forum will be apparent.”
When a person with disability engages in behaviours that put themselves and/or others at risk of harm, this is referred to as ‘behaviours of concern’.
Psychotropic medications are any drug capable of affecting the mind, emotions or behaviour. Among the types of psychotropic drugs are antipsychotics, antidepressants, and mood stabilisers.
Her brother “looked like a zombie”
Rose Atherton gave evidence at the Disability Royal Commission about the care her younger brother, Glen Hardwick, received while living in a group home located in regional Victoria.
Glen lived with an intellectual disability and resided in supported accommodation in Australia from 2013. He died, aged 37, after an allergic reaction following heart surgery.
Ms Atherton says that her brother was cheeky and liked making jokes.
“He made an everlasting connection with people he ran into and he never forgot people that he met,” says Ms Atherton.
“Glen could comprehend most things, and he had a connection also with the older generation as they would give him the time of day and have that chat with him.
“He always rang every night, mum and dad or me or my brother. And he was very much on the phone, you know, just telling us what happened or who he bumped into. He had a job at the local supermarket every Saturday morning, and he would do that come hail, snow, sun. He loved it.”
When her brother arrived at a Christmas Day gathering in 2017 looking “like a zombie”, Ms Atheron knew there was something wrong.
“There were no facial expressions. He was dribbling. He wasn’t interacting with the dogs which he normally loved. He just sat there. He just looked like an old man, and everyone actually commented that day, what’s wrong with Glen. And that’s when I said to mum, ‘We’ve got to do something here, I want the old Glen back’.”
Staff from the group home had been accompanying Mr Hardwick to his medical appointments.
Ms Atherton raised her concerns with his psychiatrist, outside of the group home, and Mr Hardwick was soon taken off the medication.
“The psychiatrist backed off the medication because he even said to me, ‘Where’s the old Glen?’”
Ms Atheron ended her submission by telling the Royal Commission that greater training needed to be given to staff to ensure they knew how to manage challenging behaviours properly.
GP calls for structural changes to health and disability services
A New South Wales General Practitioner (GP) told the Disability Royal Commission there was not a “strong evidence base” for the use of many of the psychotropic medications she sees administered to people with intellectual disability.
Dr Jane Law says that when people with intellectual disability display perceived behaviours of concern, the challenge is to avoid excessive or unnecessary use of medication in response.
“Behaviours are often due to mental health issues, communication difficulties, physical complaints or environmental concerns, which all need identifying and appropriate management,” explains Dr Law.
She described the services provided to people with intellectual disability as “compartmentalised, causing barriers to access and care”, noting this has a particularly detrimental impact on people with mental health issues and behaviours of concern.
She says some of her patients displaying behaviours of concern, such as self-harm and aggression towards others, were prescribed psychotropic medications but their medications were reduced or stopped after other health issues and environmental problems were addressed.
Dr Law provided examples of non-verbal patients, one has been found to be suffering from cataract blindness, another patient who was found to have a blocked bowel, and another who allegedly had been physically and mentally abused at a group home.
“Managing behaviours of concern including reducing or eliminating the use of psychotropic medication requires a full examination into the cause(s) of the behaviours and thus, a coordinated, well-funded and robust system, including integrated medical, psychiatric, environmental, communication and behaviour support systems”, says Dr Law.
“Such holistic care requires adequate training and specialisation for all those caring for a person with an intellectual disability.”
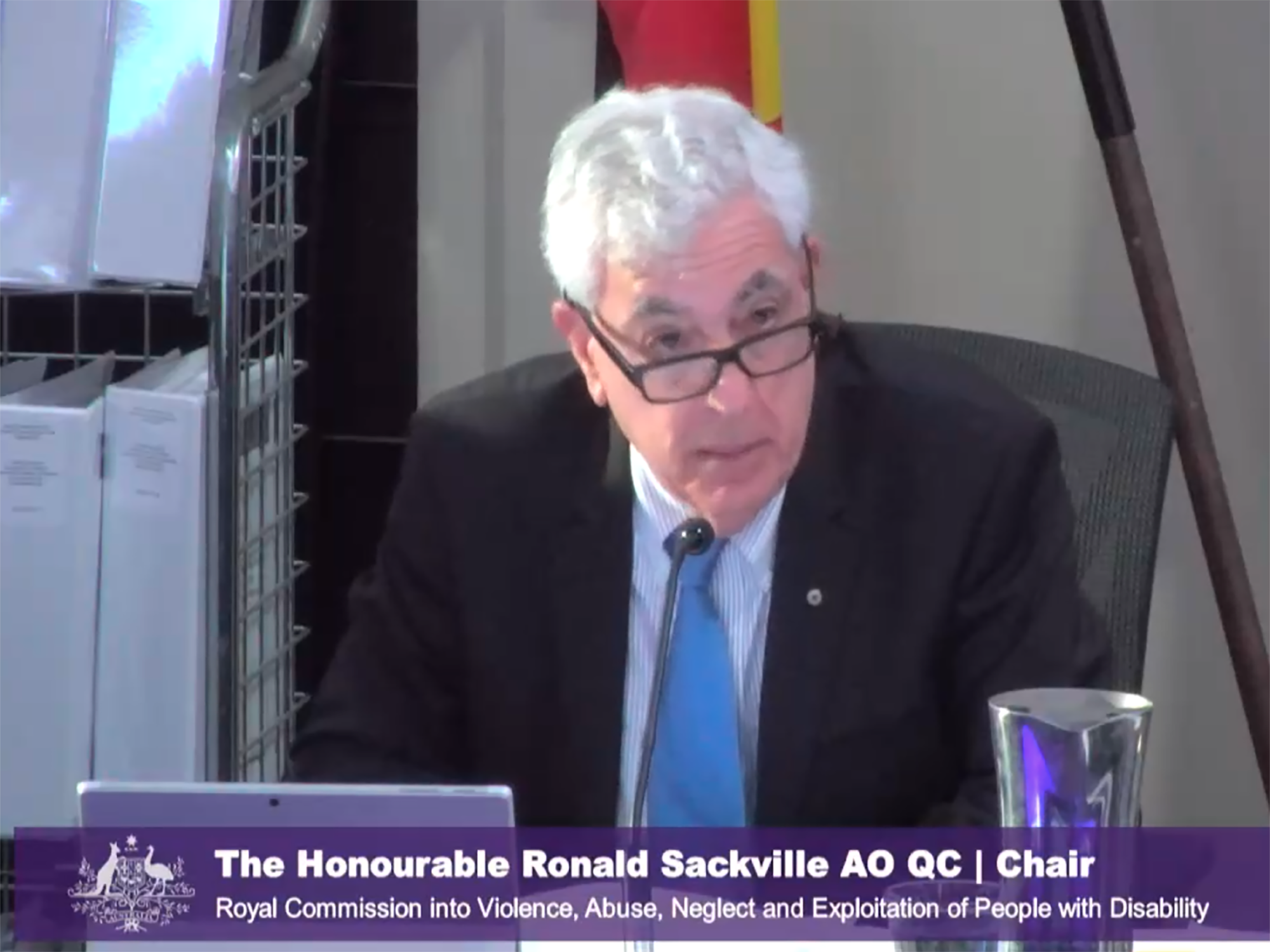
Ronald Sackville’s, Chair of the Royal Commission, closing remarks at the end of the four day hearing reiterated the need to understand how someone with intellectual disability communicates.
“Many of the witnesses explained that behaviour is a form of communication for all of us and that for people with intellectual disability or autism, their principal, and sometimes their only means of communication, is through behaviour,” states Mr Sackville.
“We, therefore, need to understand what the person is communicating and how the concerns or feelings they are communicating can best be addressed.
“In particular, we need to develop more effective mechanisms to address the physical, emotional, and environmental factors that influence a person’s behaviour and not resort to the use of psychotropic drugs as an instrument for controlling the behaviour of people with disability or people with autism.”
The Royal Commission will continue its hearings on 12 – 16 October 2020 covering, barriers to accessing a safe, quality and inclusive school education.